Let’s start with a brief (relatively) look at what happens in the skin when you get a pimple. Understanding this not only helps you to choose better topical treatments, but it also explains why I’m asking you to make certain dietary changes or take specific supplements.
Summary / TL;DR
Acne is an inflammatory disease of the skin follicles (skin pores). Each follicle is like a tube that’s lined with cells called keratinocytes. Due to various reasons, in acne-prone skin keratinocytes grow and divide faster than normal. Accumulation of keratinocytes on the walls narrows and eventually blocks the skin pore, leading to the first stage of a pimple known as microcomedo.
As sebum and dead skin cells accumulate in the blocked pore, it expands and turns into a comedo, i.e. a blackhead or a whitehead.
As the walls get thicker, red blood cells cannot deliver oxygen into the blocked pore. Low oxygen environment is ideal for acne-causing bacteria to multiply, resulting in an exponential increase in inflammation in the area and formation of an inflammatory pimple (papules and pustules). If the follicle breaks, the inflammatory material spills and inflammation spreads into the surrounding area. In the skin, you’ll see this as a large inflamed area surrounding the original pimple.
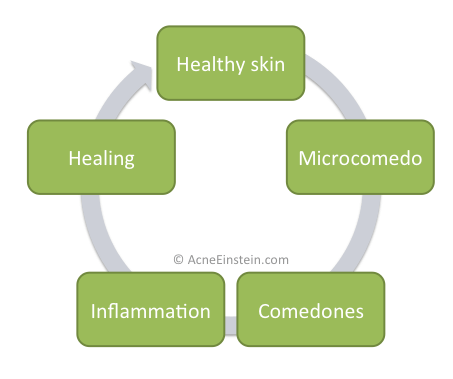
I call this progress from healthy skin pores through microcomedones and comedones into inflammatory pimples as acne cycle.
No single cause is responsible for the acne cycle, but scientists have linked several factors to various stages of the acne cycle, including:
- Deficiency in linoleic acid (LA). Sebum from acne patients has less LA than sebum from people without acne, causing a localized LA deficiency in the skin pores. LA deficiency has been linked to excess keratinocyte growth. LA deficiency also makes the immune system more aggressive; studies have shown that LA suppresses the number of free radicals white blood cells release when they encounter bacteria. Free radicals destroy the bacteria but also cause oxidative damage to the healthy cells in the area.
- Oxidative stress and lipid peroxidation. Sebum contains a substance called squalene. Oxidative damage turns squalene into squalene peroxide, a highly comedogenic substance suspected to be the trigger that kicks off the acne cycle. Sources of oxidative damage include UV radiation, air pollution, bacterial toxins or free radicals released by white blood cells.
- Insufficient antioxidants. Several studies show that acne patients don’t have enough antioxidants to protect squalene from oxidative damage. Low levels of antioxidants and higher levels of oxidative damage has been observed both in the skin and systemically in the body. Though, whether this is a cause or consequence of acne is not yet known.
- Hormones and diet. Hormones affect nearly all the factors linked to the acne cycle. They increase keratinocyte growth, boost sebum production, and regulate inflammation. Acne is usually linked to androgens (male sex hormones). But studies show that most people with acne have normal levels of androgens. New studies show that hormones insulin and insulin like growth factor-1 (IGF-1), as well as amino acid (protein) availability, regulate the sensitivity of the skin to androgens. This suggests that insulin, rather than androgens, is the most relevant hormone for acne patients.
- Stress. Neurotransmitters released during stress can cause inflammation in skin cells and increase sebum production.
- Bacteria. While no one denies that bacteria have a role in acne formation, new research shows that bacteria do not cause the early stages of the acne cycle. Bacteria exponentially increase inflammation in already-blocked pores. As such, antibacterials should be a part, but not the focus, of your acne treatment program.
The acne cycle
The graph below describes what I call as the ‘acne cycle’.
Microcomedo
The skin is mainly composed of cells called keratinocytes. The primary function of keratinocytes is to form a barrier that protects against environmental damage and bacteria. Keratinocytes also form the wall around skin follicles (pores). Due to various reasons (covered in the in-depth section) keratinocytes start to multiply rapidly, which both narrows the follicle opening and makes it more rigid; keratinocytes contain a tough protein called keratin. In medical terms, this condition is called hyperkeratosis.
The combination of dead skin cells and sebum clogs the opening of the follicle. This is your typical blocked pore, also known as a microcomedo. Microcomedones are the first stage of the acne formation process and are invisible to the naked eye.
Comedo
Attached to the skin follicle are sebaceous glands. These glands produce cells called sebocytes. You can think of sebocytes as tiny oil-filled water balloons. As they are pushed into the hair follicle, they burst and release the oil into follicle and on the surface of the skin.
The sebaceous glands are ‘dumb’ in a way that they don’t realize the follicle is blocked, and just keep pumping sebum into the follicle.
As more and more sebum and dead skin cells get pushed into the blocked follicle, it starts to expand. Much like what happens when you fill a water balloon. This ballooned follicle is called a comedo.
Some comedones have a tiny opening through which little oxygen can flow into the follicle. The resulting oxidation turns the sebum in the follicle black; creating a blackhead.
Completely blocked comedones with no oxygen are called whiteheads.
Inflammation
As the follicle expands, the walls become compacted due to increased pressure. Red blood cells have difficulties supplying oxygen through the compacted wall and the oxygen content drops.
This oxygen-poor but sebum-rich environment is ideal for the P. Acnes bacteria to thrive in, resulting in exponential growth of the bacteria. Drastic growth of the bacteria exponentially increases inflammation in the area, which results in an inflammatory pimple, also known as papules and pustules.
Sooner of later the expanded follicle bursts and spills the enclosed material into the surrounding area. You can see this as the redness and inflammation spreads around the original pimple; in medical speak this type of a pimple is called a nodule.
Healing
Eventually, the immune system clears the mess and another follicle forms in the area.
I should point out that not all of the problematic follicles go through this entire cycle. Some comedones never turn into inflammatory pimples. Likewise, studies have shown that some inflammatory pimples form from apparently healthy skin without going through the microcomedo and comedo phases.
Factors that contribute to the acne cycle
Studies have conclusively shown that there is no single factor that triggers the acne cycle. Rather, several factors come into play in different parts of the cycle, and it’s likely that these factors vary from person to person.
Here are the factors researchers believe are the most important.
Linoleic acid deficiency and sebum composition
Several studies have shown sebum composition differs between people with acne and those with clear skin. Among the most significant differences are a decrease in linoleic acid (LA) and an increase in squalene.
There’s an inverse relationship between sebum production and linoleic acid concentrations; i.e. the more sebum is produced the lower the LA concentration is. This could explain why people with acne have less LA in sebum.
Deficiency in LA causes barrier problems in the follicular duct (. Think of the skin pore (follicle) as a tube, LA deficiency causes holes to appear in the wall of the tube, and consequently makes them weaker. This makes the follicle more prone to rupture and may result in leakage of substances inside the follicle into the surrounding area. Some of these substances are inflammatory, like bacterial toxins, and likely cause inflammation in the area.
Linoleic acid can also dial down immune system reaction in the skin. LA reduces the number of free radicals white blood cells release when they come in contact with bacteria and other harmful substances in the skin. The immune system in acne patients seems to be more aggressive and this could trigger or worsen acne by releasing more free radicals (reactive oxygen species, or ROS). One paper concluded:
Our experimental results seem to reveal an involvement of neutrophil-derived ROS in the irritation and destruction of the follicular wall, which is responsible for inflammatory progression in acne.
Akamatsu, H. & Horio, T. The possible role of reactive oxygen species generated by neutrophils in mediating acne inflammation. Dermatology (Basel) 196, 82–5 (1998). https://www.ncbi.nlm.nih.gov/pubmed/9557235
Researchers also believe that LA deficiency contributes to hyperkeratinization and microcomedo formation.
Consequently, a handful of studies have shown that topical application of LA reduce acne. Results vary from 25 to 60+% reduction.
Other investigations have shown that sebum from acne patients is particularly rich in squalene, one study showed 2.2 fold increase in squalene concentration. Squalene is problematic because it’s highly sensitive to UV radiation and other forms of oxidative damage.
Oxidative stress and lipid peroxidation
Oxidative stress is one of the most important factors in acne. Oxidative stress refers to an imbalance between formation of free radicals and the body’s ability to neutralize them with antioxidants. Exposure to UV radiation, air pollution, bacteria and other harmful influences are known to produce free radicals.
A number of studies have shown that acne patients are under more oxidative stress than people with clear skin.
Due to its unsaturated structure, squalene is sensitive to oxidative damage, and following UV exposure forms squalene peroxides. This process is called lipid peroxidation, or oxidative destruction of lipids (fats).
Squalene peroxide is highly comedogenic. Animal studies show that injecting squalene peroxide into rabbit ears caused acne and that the severity of acne correlates with the degree of oxidative damage squalene had suffered.
Test tube studies have shown squalene peroxides further increase keratinocyte growth and may boost sebum production.
Many researchers believe that oxidative damage to squalene is the trigger that kicks off the acne formation process.
Emerging studies have shown that patients with acne are under increased cutaneous and systemic oxidative stress. Indeed, there are indications that lipid peroxidation itself is a match that lights an inflammatory cascade in acne. The notion that lipid peroxidation is a “starter gun” in acne is not a new one; here we review the nearly 50-year-old lipid peroxidation theory and provide a historical perspective to the contemporary investigations and clinical implications.
Bowe, W. P. & Logan, A. C. Clinical implications of lipid peroxidation in acne vulgaris: old wine in new bottles. Lipids Health Dis 9, 141 (2010). https://www.ncbi.nlm.nih.gov/pubmed/21143923
Whether squalene peroxidation is the thing that kicks off the acne cycle remains to be seen, but there’s no doubt that it plays a significant role in acne. As evidenced by numerous studies that show topical antioxidants reduce acne as much as benzoyl peroxide and topical antibiotics.
The problem of oxidative stress is not restricted to the skin. Several studies indicate that:
- Acne patients have lower levels of antioxidants and vitamins as compared acne-free peers.
- A Clear correlation between acne severity and oxidative stress has been found. People with moderate/severe acne have lower levels of antioxidants and higher levels of substances that indicate oxidative stress and inflammation.
- Treatment with antioxidant supplements has been shown to reduce acne.
Researchers have yet to understand how oxidative stress outside of the skin affects acne. One explanation is that increase in oxidative stress depletes antioxidant reserves and leaves the skin vulnerable to oxidative damage.
Another possibility is that the immune system in acne patients is more aggressive and produces more free radicals (and thus also demands more antioxidants).
Regardless, it’s clear that at least some acne patients have higher levels of oxidative stress and that addressing it will likely help the skin.
A 2012 review paper on the role of oxidative stress on acne concluded the following:
Increasingly, studies suggest that patients with acne are under increased amounts of cutaneous and systemic oxidative stress. They demonstrate increased markers of oxidative damage, and appear to consume antioxidants at a faster pace than their acne free peers. Furthermore, recent evidence suggests that oxidative stress and inflammation might actually precede all of the other steps in the sequence of acne pathogenesis.
Bowe, W. P., Patel, N. & Logan, A. C. Acne vulgaris: the role of oxidative stress and the potential therapeutic value of local and systemic antioxidants. J Drugs Dermatol11, 742–6 (2012). https://www.ncbi.nlm.nih.gov/pubmed/22648222
Hormones
Just about everyone understands hormones affect acne. There’s no controversy about this in the medical literature. I’ll go more into details of how hormones affect acne in the in-depth section, but here I want to bring your attention to a point that’s often missed.
Acne is most often linked to androgens or male sex hormones. And people make the assumption that having hormonal acne means your androgen levels are too high. This is demonstrably not true. Several studies have compared androgen levels between women with and without acne. These studies clearly show that women with acne, on average, have slightly higher levels of various androgens, but the differences are not huge and most hormones remain within the normal range.
The one exception to this is DHEA, a relatively weak precursor hormone to testosterone and DHT. Studies show a strong correlation between DHEA levels and acne, and just about every study I looked at showed that women with acne have higher levels of DHEA than women without acne. The skin converts DHEA into testosterone and DHT; the two hormones that most actively stimulate skin cell growth and sebum production.
In other words, the blood levels of these hormones are usually not the problem. Of course, there are exceptions, such as women with polycystic ovary syndrome. In such cases, elevated androgen levels are a part of the problem. But for the majority of people struggling with adult acne, blood levels of androgen hormones aren’t the real problem. The way your skin reacts to them is.
Pioneering work by Dr. Bodo Melnik has shown that the skin contains two substances that regulate the skin’s responsiveness to androgen hormones. These are:
- Forkhead box protein O1 (FOXO1)
- Mammalian target of rapamycin (mTOR)
Both of these substances regulate cell growth and other factors in response to nutrient availability and hormone levels. Exactly how these substances work in the skin is both complicated and not relevant to our discussion.
What matters is that these substances affect nearly all the proximal causes of acne, including:
- Regulate the growth of both keratinocytes and sebocytes. As we discussed earlier, excess keratinocyte growth leads to blocked pores, and sebocyte growth increases the amount of oil your skin produces.
- Regulate androgen receptor sensitivity in the skin.
- Regulate the immune system response in the skin.
- Control the number of antimicrobial substances the skin produces.
FOXO1 and mTOR respond to:
- Levels of the hormones insulin and insulin like growth factor-1 (IGF-1).
- The amount of available amino acids, especially leucine.
- Energy balance, i.e. whether you are eating more or fewer calories than you burn.
FOXO1 and mTOR oppose each other, but for the sake of simplicity, think of their combined effect like a dimmer switch. As the above three factors increase; as insulin and IGF-1 levels increase, as more amino acids are available, as you consume more calories than you burn, the dimmer switch increases many of the proximal causes of acne.
The combined effect of FOXO1 and mTOR explains many things, including:
- Why people with normal androgen levels still get hormonal acne.
- Why insulin-lowering drugs, and diets that reduce insulin-spiking foods, help acne.
- Why dairy products are so bad for the skin. Milk can spike insulin levels as much as white sugar does, and dairy proteins contain more leucine than other protein sources. Consuming milk creates a dangerous combination of high insulin and leucine levels, a condition that’s known to fully open the regulatory ‘dimmer switch’ of FOXO1 and mTOR.
Stress
Most acne patients intuitively know that stress makes acne worse. And yet, there’s almost no research into the connection. As far as I can tell, only two studies have looked into whether acne gets worse during stressful times. Both studies were done on students and compared examination period (high stress) to summer holiday (low stress), and both studies showed the students had more acne during the examination periods.
Stress can affect acne both directly and indirectly.
- Stressful and anxiety-producing situations trigger the release of a neurotransmitter substance P (SP). SP can trigger an inflammatory response in skin cells, and there’s some evidence to suggest it increases sebum production. Nobody has studied what SP does in people with acne, but injecting SP into the skin of psoriasis patients triggered psoriatic flares.
- Stress is known to affect negatively just about every aspect of gut health.
- Stress causes inflammation in the body.
- Stress triggers the release of DHEA hormone, which acts as a sort of feel good hormone and buffers you against the harmful effects of stress. Unfortunately, as we saw in the discussion about hormones, DHEA is one of the principal hormones in acne. The skin contains all the enzymes required for converting DHEA into testosterone and DHT, both of which strongly stimulate skin cell growth and sebum production.
The good news is that these responses are not set in stone. Doing self-compassion exercises and building emotional resilience can significantly reduce the harmful effects of stress. Please see the emotional-type acne section to get started.
Bacteria and other pathogens
There’s no doubt that bacteria are involved at some stages of the acne cycle. Contrary to earlier ideas, bacteria doesn’t seem to cause, or trigger, the acne cycle. However, once a comedo has formed, colonization of the blocked pore with bacteria exponentially increases inflammation in the area and turns it into an inflammatory pimple.
Bacteria are probably not involved in the initiation of comedones. Electron microscopy of early noninflamed lesions taken from prepubertal and early pubertal individuals has demonstrated few or no bacteria…
However, bacteria, particularly Propionibacterium acnes, are likely involved later in comedogenesis.
Cunliffe, W., Holland, D. B. & Jeremy. Comedone formation: Etiology, clinical presentation, and treatment. Clin Dermatol22, 367–374 (2004). https://www.ncbi.nlm.nih.gov/pubmed/15556720
For this reason, it’s important to include antibacterial products into your skin care routine.
Propionibacterium acnes is not the only pathogen that causes skin problems. A fungus called Malassezia can cause skin problems that are often mistaken as acne, but this is something we’ll talk more in the infectious-type acne page.
Garden hose analogy
Here’s an analogy that ties all of this together. Think of a thin garden hose, like a hose that’s made of thin rubber and will burst if the water pressure gets too high. Think of your skin like this hose. If it burst, you’ll get acne.
Hormones, oxidative stress, and inflammation are the water that goes through the hose. Per se, they don’t cause acne, but the higher the water pressure, the more likely it is that the hose will burst.
There are also things that weaken the hose. An old hose that’s left out in the sun becomes fragile and will break easier than a new hose. Things that weaken the hose include genes that predispose you to acne, exposure of the skin to UV radiation and other forms of oxidative damage, bacteria in the skin, linoleic acid deficiency, etc.
Acne is a combination of all of these factors. Usually, there’s not a one single thing that causes it. Similarly, getting over it comes down to strengthening the hose and doing your best to reduce the amount of water you put it.

