Another group of hormones linked to acne includes growth hormone (GH), insulin and insulin-like growth factor 1 (IGF-1). On this page, I’ll focus more on insulin and IGF-1 because they are more amendable to diet and lifestyle interventions.
Insulin is a metabolic hormone that regulates the storage of carbohydrates, fats, and amino acids. The primary functions include absorption of glucose from the blood to muscle cells and storage of fats into fat tissue. Insulin-like growth factor 1 is a growth hormone with a similar molecular structure to insulin.
GH, insulin, and IGF-1 affect acne in two ways. Acting alone, they can stimulate sebum production and skin cell growth much like androgens can. Cell culture studies have shown that growth hormone has the most profound effect, followed by IGF-1 and then insulin. Studies have also shown they add to the effect of androgens. When skin cells are exposed to androgens and GH/insulin/IGF-1, they produce more sebum than when exposed to either group of hormones alone. (source)
Much like androgens, IGF-1 is required for the development of acne. A 2011 study on Laron syndrome patients, who are deficient in IGF-1, showed very low rates of acne. Furthermore, a large dose of IGF-1 resulted in acne and hyperandrogenism in half of the female patients, but acne disappeared after lowering the IGF-1 dose.
From the study conclusion:
This study demonstrates for the first time that serum IGF-1 deficiency prevents the occurrence of acne. The findings suggest that an interaction between IGF-1 and androgens is necessary for the development of acne.
D. Ben-Amitai1, Z. Laron. Effect of insulin-like growth factor-1 deficiency or administration on the occurrence of acne. Journal of the European Academy of Dermatology and Venereology. Volume 25, Issue 8, pages 950–954, August 2011. https://www.ncbi.nlm.nih.gov/pubmed/21054577
One paper describing Laron syndrome case reports clearly illustrated the role IGF-1 plays in stimulating androgen release and causation of acne.
During the administration of IGF-I in what we subsequently discovered to be excessively high doses, four out of the six developed, in a progressive manner, increased serum levels of testosterone, and D4-androstenedione which led to clinical signs of oligomenorrhoea and acne.
Klinger, B., Anin, S., Silbergeld, A., Eshet, R. & Laron, Z. Development of hyperandrogenism during treatment with insulin-like growth factor-I (IGF-I) in female patients with Laron syndrome. Clin. Endocrinol. (Oxf) 48, 81–7 (1998). https://www.ncbi.nlm.nih.gov/pubmed/9509072
As the study mentioned, insulin and IGF-1 also interact with androgen hormones, which is the second way they affect acne. I like to call them booster hormones because they appear to ‘boost’ the acnegenic effect of androgens.
Research has shown the following interactions between androgens and IGF-1.
- IGF-1 is a key hormonal regulator of androgen synthesis in the adrenals, and several studies have found correlations between IGF-1 and DHEAS levels. DHEAS, as we saw on the page on androgens, can be converted to testosterone and further to DHT in the skin.
- Insulin and IGF-1 inhibit the liver’s production of sex hormone binding globulin (SHBG). SHBG binds to testosterone and other androgens in the blood, and while bound to SHBG, they are not bioavailable. Decrease in SHBG means increased amount of free (bioactive) androgens and a greater androgen effect on acne.
- Insulin and IGF-1 affect the ‘master regulator’ proteins forkhead box protein 01 (Fox01) and mammalian target of rapamycin (mTor) in the skin. You can think of the combined effect of FoxO1 and mTor like a dimmer switch that regulates how the skin responds to androgens. Higher levels of insulin and IGF-1 dial up this dimmer switch and make your skin more sensitive to androgen hormones.
- Cell culture studies have shown that IGF-1 increases 5-alpha reductase enzyme in a dose-dependent manner. This means more DHT to stimulate the skin and sebum cells.
For all these reasons, studies have found that IGF-1 levels correlate with sebum production, skin pore size, and acne lesion count in women. In men, IGF-1 correlates with some of the androgen hormones. (source)
All this evidence points to the inescapable conclusion that insulin, IGF1 and androgens conspire to make a real mess of your face. Before moving on, let’s talk briefly about insulin, which, it turns out, is one of the few hormones in this equation you have real control over.
Insulin
All this talk about androgens and IGF-1 is nice on paper, but not very practical. As there’s little you can do to influence the levels of those hormones directly. Not so with insulin. With diet and lifestyle choices you have lots of control over your insulin levels. And that turns out to be the saving grace here, as insulin acts as a sort of a cornerstone hormone in all of this.
According to Wikipedia, approximately 98% of the IGF-1 is bound to insulin-like growth factor binding proteins (IGFBP). As it was with androgens, bound IGF-1 is not bioactive. It circulates in your blood without affecting anything. It’s there as a reserve that the body can quickly draw from.
Insulin increases IGF-1 and reduces IGFBP levels. In other words, insulin both increases IGF-1 blood levels and its bioavailability. So chronically high insulin levels mean more acne-boosting IGF-1. In contrast, cutting energy and protein intake has been shown to reduce IGF-1 levels. (source)
Several studies have shown that the transient insulin resistance (and thus elevated insulin levels) during puberty is associated with higher IGF-1 levels (source, source). Adult patients with metabolic syndrome show both high insulin and high IGF-1 levels.
All this fits in nicely with what we know about acne and insulin resistance.
Insulin resistance
Insulin resistance is a condition in which the cells’ response to insulin is hindered, and the pancreas has to compensate by releasing more insulin.
A 2012 Italian study looked at 22 young men with acne and compared their blood sugar metabolism to 22 healthy controls.
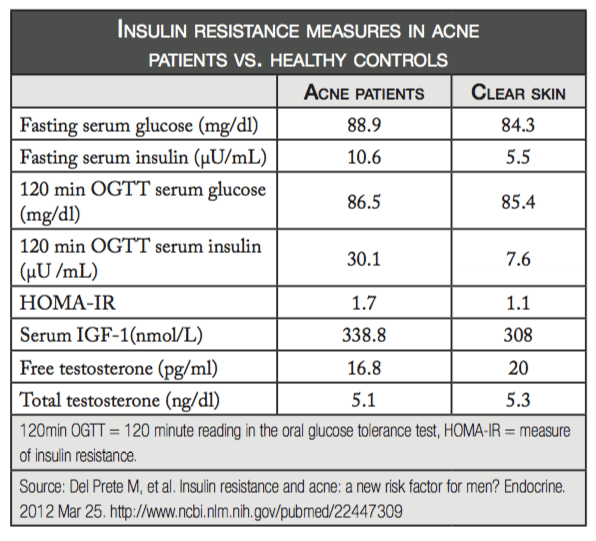
These data clearly show insulin resistance in acne patients. While the difference in blood glucose (blood sugar) levels is minimal, acne patients require significantly higher insulin levels to achieve them. The difference in 120-minutes oral glucose tolerance tests (OGTT) is especially striking, with acne patients showing almost 400% higher insulin levels. Acne patients also had about 10% higher IGF-1 levels.
Interestingly, people with clear skin had somewhat higher testosterone and free testosterone levels, which goes to show how complicated the relationship between acne and hormones is.
To date, five studies have looked at whether people with acne have insulin resistance. 4 showed people with acne are insulin resistant and/or have higher insulin levels than comparable people without acne.
I should say that we don’t have enough data to show that insulin resistance is a problem for every acne patient, but these studies show it certainly plays a part, especially given how insulin resistance ties in with all the other hormonal factors discussed here.

