If you’ve experienced acne lately, you know how hard it can be on your health and appearance. Maybe you’re one of the lucky ones who hasn’t had a breakout since you were a teenager. But, now that you’re pregnant, all of a sudden your face or back is now covered with pimples.
What happened to that clear skin you were so used to? Let’s take a look at what happens to your body when you’re pregnant. Can it actually cause acne?
Does pregnancy cause acne?
Up to 42 percent of women can have acne during pregnancy. In addition, nearly 50 percent of pregnant women visit skin clinics with inflammatory skin problems including psoriasis, rosacea, and eczema. This increase in skin problems can occur due to increased oil gland activity and hormonal changes during pregnancy. The risk is even higher among women who have a history of acne or oily skin.
Acne can develop or become worse during any period of pregnancy. Although it is commonly believed that acne is the most common during the first and second trimester, recent studies suggest it is more likely to occur during the third trimester. One small study found that pregnant women had the highest number of facial acne during the second trimester.
What exactly causes pregnancy acne?
Pregnancy acne can result primarily due to two reasons:
- Increased activity of oil glands. Oil glands called eccrine and sebaceous glands tend to have higher activity during pregnancy. Typically, this occurs during the last few months of pregnancy, according to a study in the journal Clinical Obstetrics and Gynecology.
- Increased androgen levels. Typically, this occurs during the third trimester. Increased androgen hormones can lead to increased oil gland activity and lead to a vicious cycle. In addition to increasing the risk of acne in the mother, transfer of androgens from mother to the unborn baby can lead to acne in newborns, which is called acne neonatorum. However, it is usually mild and resolves on its own within a few months.
While clinical studies are the cornerstone of evidence, it is still hard to discount anecdotal evidence. For instance, some reports say if you do not have acne in early pregnancy, it is less likely that you will get it in the second or third trimesters. For the most part though, acne can occur at any time during pregnancy and is highly individualized.
Studies also reveal that changes in acne during pregnancy can occur through additional mechanisms other than hormonal changes and increased activity of oil glands. Inflammation of the hair follicle, also called folliculitis, can contribute to the appearance of acne although it is rare.
Interestingly, while overactive oil glands may be bad news for some women with acne, for others, it might actually help improve skin and produce that pregnancy glow. Still, it’s a toss up with the current evidence available.
Acne treatment during pregnancy
Treating acne in pregnancy is invariably tricky given the potential risks to unborn baby due to medications used by pregnant women. While some treatments are safe and effective, others can cause serious adverse effects to the unborn baby.
Here are some general guidelines to follow when you have pregnancy acne.
- Wash your skin twice daily with lukewarm water and gentle cleansers. Do not use scrubs or any cleanser that contains beads. Even though the beads may be tiny, they can cause skin irritation and increase inflammation.
- Experts at the American Academy of Dermatology (AAD) suggest starting with topical medications such as OTC glycolic acid and facial washes if needed.
- Protect your skin from potential sunlight-induced pigmentary damages with a broad-spectrum sunscreen with SPF of 30 or more.
- Regularly clean your hair with a mild shampoo. This might help reduce acne around your hairline.
- Avoid picking your acne.
- Avoid dairy and high-sugar products as they might make your condition worse.
If the symptoms do not improve with these approaches, you should consult a doctor. Your doctor may prescribe topical antibiotics including erythromycin, clindamycin, azelaic acid, or metronidazole to help fight stubborn acne.
Among these topical medications, experts say azelaic acid is perhaps more advantageous in treating pregnancy acne because it has an added benefit of improving blemishes.
If your acne does not respond to topical antibiotics or becomes worse, the doctor may prescribe oral azithromycin, erythromycin, or cephalexin. All of these oral antibiotics have an excellent safety profile for use in pregnancy. Rarely, for severe cases, they may want to use oral corticosteroids to help with inflammation.
After your visit with a dermatologist, your treatment regimen may look something like this:
- Treatment in the first trimester – Topical treatment with benzoyl peroxide or azelaic acid. If the condition does not improve, your doctor may prescribe oral azithromycin or clarithromycin.
- Treatment after the first trimester – Oral erythromycin. It is generally considered effective and safe when used short term (less than a few weeks). Because erythromycin is highly processed in the liver, those with liver problems may want to avoid it.
- Second-line treatment – Narrowband ultraviolet B phototherapy. According to experts, red and blue light phototherapy are safe for treating acne that is resistant to topical prescription or over-the-counter medications. Remember, your insurance may not cover such light treatments.
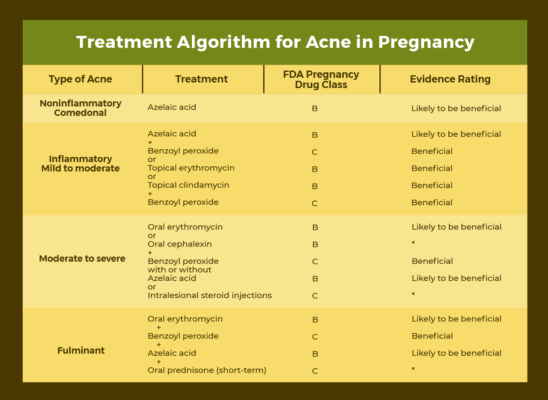
The following table gives an algorithm for treating pregnancy acne.
Other possible acne treatments
In addition to antibiotics and topical medications, one study shows that taking a zinc supplement, particularly, zinc gluconate might be a safe alternative for both pregnant and breastfeeding women. However, it primarily benefits those pregnant women who already have a zinc deficiency (which is estimated to be about 80% of pregnant women around the world). The current recommended dietary allowance for zinc during pregnancy is 11 mg/day.
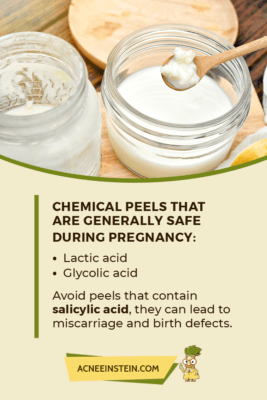
Chemical peels that use lactic acid and glycolic acid are generally safe. While salicylic acid peels can help treat acne and decrease oily skin, it is not recommended in pregnant women. Peels that contain salicylic acid can lead to miscarriage and birth defects especially if a large area of skin is treated.
Acne treatments to avoid during pregnancy
The American Academy of Dermatology (AAD) strictly prohibits the use of the following medications during pregnancy:
Retinoids including Isotretinoin
Brands: Absorica®, Amnesteem®, Claravis®, Myorisan®, Sotret®, and Zenatane™
Isotretinoin has severe teratogenic effects, which means it can affect the development of an unborn baby when used by a pregnant woman. The risk is even higher when you take it in the first trimester.
Babies exposed to isotretinoin in the mother’s womb can have various abnormalities that involve the central nervous system, head, face, and heart. Examples include: small or no ears, narrowed external ear canal, widely spaced eyes, fluid in the brain, and learning disabilities.

Tazarotene
Brands: Avage®, Fabior®, Tazorac®, and Zorac®
This topical medication belongs to the “retinoid” class of anti-acne drugs and carries similar risks to the fetus. Though the risk of birth defects is higher with oral use of retinoids, topical retinoids can also cause defects after absorption through the skin. Therefore, it’s best not to risk it and avoid retinoids altogether.
Spironolactone
Brand: Aldactone®
While spironolactone can help decrease androgen levels and improve acne, it is not generally recommended for pregnant women. Studies in animals have shown that spironolactone can cause fetal abnormalities, such as feminization of the male fetus.
Note: If you are taking other medications for acne, make sure to check the label for pregnancy information. Oftentimes, drugs will be assigned a pregnancy category such as A, B, C, D, or X, with A being the least harmful and X being the most harmful.
Here is a table where you can find the medications that you can or shouldn’t use during pregnancy.

See the table below to find the meaning of a drug’s pregnancy category.

Acne after pregnancy
So you’ve finally delivered your baby and all is well. You may be hoping for a fast recovery into breastfeeding mode. Now, your skin can snap back to what it was before the hormones, right? Unfortunately, that’s not always the case.
As with acne in general, it is important to continue taking care of your skin. Don’t immediately drop the skin care regimen you’ve been following during your pregnancy. Your skin still needs that extra care to continue fighting acne, especially if it’s still severe.
If you were put on any short-term medication treatments, ask your doctor about discontinuation and next steps. Also, if you continue using any acne medication, check to see if they are safe during breastfeeding.
How long does pregnancy acne last?
It’s very hard to tell how long you will have to struggle with those annoying zits after delivery. You will likely get rid of them once the hormones return to normal. Because every woman is different, it could take a few weeks or even months before hormones reach their pre-pregnancy levels.
Once your hormones balance out, you should notice some improvements in your skin. For those women who had acne before the pregnancy, unfortunately, you may be more prone to get it again down the line.
Acne during breastfeeding
Acne during breastfeeding may not be as common as pregnancy acne. However, nearly 20 percent of women experience acne during the first five weeks after delivery.

According to Dr. Leslie Baumann, a board-certified dermatologist, New York Times best-selling author and CEO of Baumann Cosmetic & Research Institute in Miami, the best treatment for breastfeeding women is,
“a combination of blue light treatments, a 2 percent salicylic acid cleanser, and a 5 percent benzoyl peroxide gel or lotion is the best treatment for acne in breastfeeding women.”
Other options for acne treatment during breastfeeding include:
- Oral tetracycline
- Topical antibiotics
- Azelaic acid
- Glycolic acid
- Lactic acid
- Vitamin C
- Oral contraceptives, in some cases.
In addition, Dr. Baumann recommends getting sufficient quality sleep and avoiding dairy and high-sugar foods.
Milk is a great source of calcium and avoiding it during pregnancy can affect the development of your baby’s teeth and bones. Thus, you should go for an alternative source of calcium such as almonds, broccoli, edamame, chickpeas, pinto beans, tofu, spinach, and calcium-fortified foods. You might opt for a calcium supplement after consulting with your doctor. In addition, yogurt may be less likely to cause acne problems compared to milk.
Is acne an early sign of pregnancy?
Increased hormone levels and overactive oil glands could cause acne breakouts during pregnancy. However, acne itself is not a sure sign to indicate that you are pregnant. The only safe way to tell if you are pregnant is to take a pregnancy test.
Can pregnancy acne tell the gender of your child?
The effect of fetal genders on pregnancy acne is not clear. Scientists have not yet found a link between fetal genders and the plasma level of androgens, the major hormones behind your skin breakouts.
Interestingly, a 2016 study found higher acne severity during the second and third trimesters in women with a female gendered fetus. The study was observational and involved only thirty-five cases. Thus, conclusive results are not available at the moment.
Conclusion
Overall, getting acne when your pregnant can be disheartening, especially when you already have the added stress of other pregnancy symptoms. It can be tough to manage your skin care on top of everything else. But, as we’ve discussed here, it’s just as important if you want to maintain that pregnancy glow.
Hopefully, you now have a better understanding of skin changes you might experience during pregnancy. By utilizing some of the tips we’ve discussed here, you’ll find that there are plenty of options to take care of acne. Just make sure you follow up with your doctor to ensure your pregnancy goes well with whatever you decide.


